1 : Why a total hip replacement?
As a rule, a total knee replacement is considered when medical methods of treating osteoarthritis have failed to provide the desired relief (anti-inflammatory drugs, chondroprotectors, viscosupplementation and physical treatment)
This osteoarthritis is generally the consequence of wear and tear of the joint, generally related to age and possibly to family or genetic factors. It can also be the consequence of the after-effects of an accident or necrosis.
The aim of this operation is to improve your quality of life by :
• Pain relief
• Restoring functional mobility
• Correction of angular deformities and removal of lameness (correction of length inequality is not usually possible unless it is due to a significant angular deformation)
• Maintaining the result in the long term
Generally, this operation is intended for patients over 50 years of age, whose osteoarthritis of the knee causes functional problems and a significant symptomatic impact. It can also be performed on younger patients, each case being different, only your surgeon is entitled to judge the necessity of this operation according to the seriousness of your problems.
2 : Description of the prosthesis
When conservative treatment no longer allows for a reduction in pain, your surgeon will suggest a total knee prosthesis. The surgical intervention consists in replacing the joint while preserving the collateral ligaments.
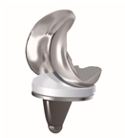
The surgeon will replace the entire joint surfaces of the femur, tibia and patella with a total prosthesis consisting of three different implants:
• The femoral prosthesis will slide and roll on the polyethylene tibial tray.
• The tibial prosthesis which itself consists of two parts:
• A metal plate anchored in the tibia.
• A rotating or fixed polyethylene platform that rests on the metal tibial tray.
• Patella prosthesis: made of polyethylene, it is not systematically fitted, depending on the wear of the patella and the type of prosthesis used.
Generally metal implants are made of ChromeCobalt (medical stainless steel), however this type of alloy contains traces of Nickel, in case of allergy to Nickel, the use of titanium implants is possible.
3 : Description of the surgical procedure
The proposed operation will be performed under general or local anaesthesia, as agreed with your anaesthetist.
You will be positioned on your back on the operating table to allow the best access to the operated knee.
After exposing the joint, the surgeon will re-cut the distal end of the femur and proximal end of the tibia, to fit the prosthetic components with either custom-made cutting guides ( MyKnee ) or with the help of the robot ( Rosa ).
These will be implanted, with or without cement, depending on the bone quality and the operator’s practices. The duration of the operation can vary between 1 and 2 hours; you will then be taken to an observation unit until you recover from anaesthesia and your vital parameters are stable (generally 24 hours of observation are necessary for your safety).
4 : Risks and complications
As a matter of principle, any major surgical operation involves general and specific risks. The surgical team implements the most appropriate care in order to reduce the risks of complications.
The general risks are the following:
- Thrombo-phlebitis
- Pulmonary embolism
- Infections
The prescription of anticoagulant drugs significantly reduces the risk of phlebitis and pulmonary embolism.
Antibiotics will also be given as a preventive measure to reduce the risk of infection. However, after your discharge from the clinic, the appearance of new pain, swelling and redness in the operated area, discharge from the scar or unexplainable fever should be reported to your surgeon as soon as possible.
5 : Pre-operative physiotherapy sessions
Some surgeons will prescribe a few sessions of physiotherapy before the operation to anticipate your apprehensions, prepare you for the use of the canes and teach you certain exercises.
However, if these sessions do not take place, do not worry, your physiotherapist will take the time to teach you the correct movements after the operation. Some technical aids may be useful.
Anticipate and familiarise yourself with this new equipment:
- Canes: these are the essential aids at the beginning of your convalescence. There are foams to place on the handles to soften the support.
- Toilet seats can be useful if your toilet is too low (or if you are tall) and you have difficulty getting up. They are available with handles.
- The wall-mounted handle for getting up from the toilet.
- The bath board: if you only have a bathtub, it can make it easier to get in. Just sit on it and swivel.
- Long tongs: can help you get dressed, pick up an object from the floor, etc.
- The long-handled shoehorn.
- Sock threader: if you have difficulty reaching your feet, it makes it easier to put on socks.
How long will I keep my two sticks?
The use of the canes is usually for four to six weeks. The length of time will be determined by your surgeon depending on your weight and bone quality.
When can I drive my car?
In general, you can drive a car as soon as you stop using canes, i.e. 4 to 6 weeks after the operation. However, if you are using an automatic car and have had surgery on your left knee, your doctor may allow you to drive sooner.
When can I start working again?
This will depend primarily on the type of work you do. In the case of work requiring physical activity, the period of absence from work will be at least 2 to 3 months.
In the case of sedentary work this period could be shortened to one month or less.
When can you take a bath?
Initially, showers should be taken or a bath board used.
In general, at six weeks, movement is free and bathing in the conventional way is allowed.
For the first 2 weeks you will have a waterproof dressing which allows showering only. Once the wound has healed, exposure to water is no longer a problem. However, getting in and out of the bathtub is usually a problem for the first 6-8 weeks.
Why is my leg more swollen now that I’m home?
At the Clinic your activity was well ordered with regular breaks where your legs were elevated. At home, you will tend to stay up and active for longer. Remember to take breaks and elevate your legs.

